Your next hire is out there for as low as $10.45/hr USD.
We'll help you hire an Insurance Claim Processor for significantly cheaper than hiring a US employee.
or 📞 call our office anytime, (860) 500-1469

Why hire with The People Company?
Low cost by hiring from the Philippines and Latin America
Your company's next insurance claim processor lives in the Philippines or Latin America, but has a great understanding of Western work culture!
Speaks incredible English
All of our hires speak English at a C2 level or above -- the highest level of qualification provided by the Cambridge Assessment.
Years of experience being an insurance claim processor
The average candidate we place has 7+ years of experience working for US companies as an insurance claim processor. You'll get someone who can hit the ground running!
or 📞 call our office anytime, (860) 500-1469
Stop overpaying for labor, and come join The People Company!
🤢 $4,500.00 USD per month
average 🗽 US salary
🇵🇭 $1,840.00 USD per month
average Philippine salary for insurance claim processors
🇻🇪 🇦🇷 🇲🇽 $2,208.00 USD per month
average LatAm salary for insurance claim processors
From $10.45/hr, all-in. No upfront fees, our fee is included in the rate.
$0 – your new hire’s first week. We pay their salary while you get comfortable with them.
$0 – payroll tax, workman’s comp, unemployment insurance, benefits, etc. or anything else you have to pay with a US employee.
$0 – onboarding fees. We give each customer personalized, white-glove service.
$0 – recruiting fees. We seek out, interview, and vet your new hire for free.
$0 – payroll & global compliance. We take care of all of the headache that comes w/ hiring someone internationally.
$0 – unlimited support. Get unlimited phone & email support with managing/onboarding your hire.
or 📞 call our office anytime, (860) 500-1469
How does it work?
1. Hop on a call
We’d hop on a phone call and get a little more context as to what you and your team are spending their day on, and what you’d like to outsource.
We’ll use this data to find the perfect assistant (or assistants, depending on your org size!)
Timeframe: 1-2 days
2. We headhunt
Our headhunter would take the data from our phone call and find candidates from our talent pool with experience in supporting teams in your industry.
Bonus points for experience with your CRM and tools, and a great culture fit.
Timeframe: 2-3 days
3. Interview & trial
We’ll present three compelling candidates and you can interview as many of those as you’d like. When you’ve found a great assistant, we will pay their first week’s salary so you can be confident they’ll be a value-add.
If they’re not a good fit, we’ll work night and day to find someone who is.
Timeframe: 7 days
Expect insurance claim processors that can fit this job description:
They'll have proficiency in these tasks:
-Verify the accuracy of claim documentation, including medical records, police reports, and other supporting documents.
-Communicate with claimants, medical professionals, or other third parties to gather additional information or clarify details related to the claim.
-Input claim information into the insurance company’s system, ensuring all data is accurate and up to date.
-Evaluate claims against policy terms and conditions to determine the extent of coverage and payout amounts.
-Approve or deny claims based on the findings from the review, ensuring decisions are compliant with company policies and regulations.
-Calculate and process claim payments, ensuring timely and accurate disbursement to policyholders or service providers.
-Investigate potential fraudulent claims by reviewing details and comparing them with known fraud indicators.
-Maintain organized records of all claims processed, ensuring easy retrieval for future reference or audits.
-Collaborate with the legal or fraud investigation teams when handling disputed or complex claims.
-Provide claimants with regular updates on the status of their claims and address any questions or concerns they may have.
-Ensure compliance with all state and federal regulations related to insurance claims processing.
They'll know how to handle these responsibilities:
-Communicate with claimants and third parties to gather any necessary additional information or documentation.
-Input and maintain accurate claim data in the company’s claims management system.
-Evaluate claims and determine approval or denial based on policy coverage and company guidelines.
-Process and calculate claim payments, ensuring they are disbursed in a timely and accurate manner.
-Identify and report any potential fraudulent claims for further investigation by the appropriate team.
-Provide claimants with updates on their claims and assist with any inquiries or issues they may have.
They'll have these qualifications:
-Strong attention to detail to accurately review and process insurance claims.
-Good communication skills for effectively interacting with claimants and internal teams.
-Proficiency in claims management software and basic computer skills.
-Knowledge of insurance policies, regulations, and claims procedures.
-Analytical and problem-solving skills to evaluate claims and handle complex cases.
-Ability to manage multiple tasks and work under tight deadlines in a fast-paced environment.
They'll be proficient in your 'tech stack', which may include:
or 📞 call our office anytime, (860) 500-1469

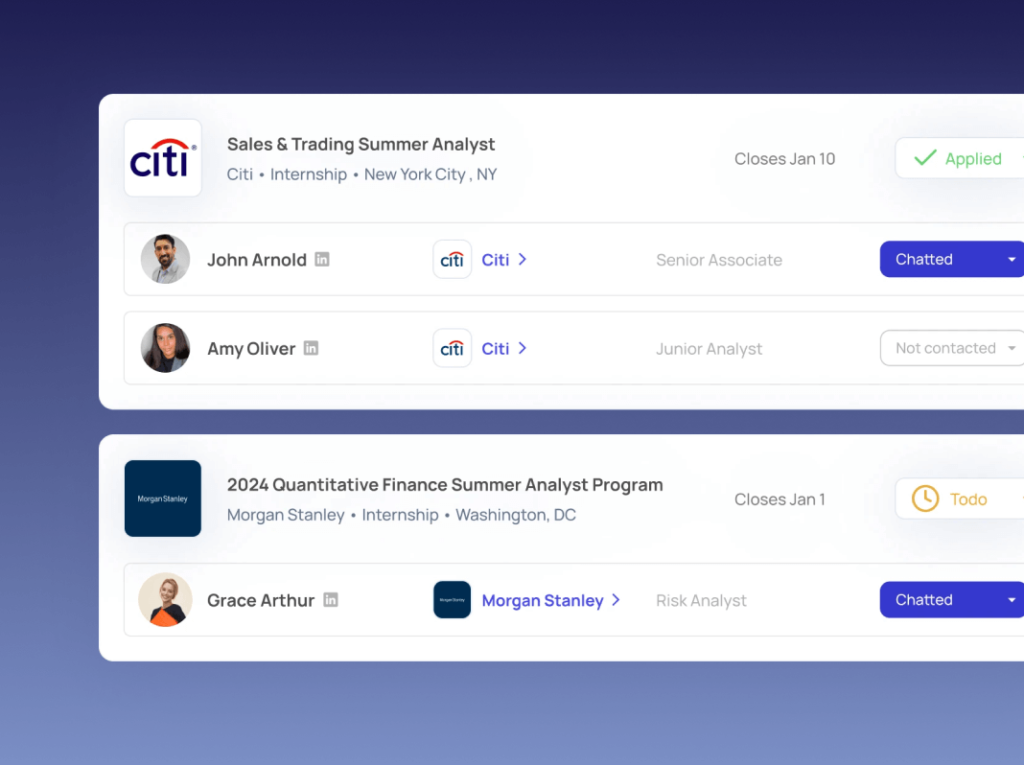
RecruitU hires great team members at 18% of the US cost with The People Company
RecruitU used The People Company to place Rico, an administrative assistant who took off vital business processes. This saved the founders a ton of time and allowed them to focus on ‘more important’ work.
Brooks Gammill, Co-Founder at RecruitU
⭐⭐⭐⭐⭐ "Hiring Rico through The People Company has been an absolute game changer. Since onboarding Rico I can now spend more time on sales and prospecting knowing that my all my administrative tasks are dealt with"